Water and blood plasma are two important components of the human body.
Water makes up about 60% of the human body and is essential for many physiological processes such as regulating body temperature, transporting nutrients and waste products, and cushioning joints and organs.
Blood plasma, on the other hand, is the yellowish fluid component of blood that makes up about 55% of total blood volume. It carries important substances throughout the body, including red and white blood cells, hormones, vitamins, and minerals. Blood plasma also helps regulate blood pressure and is involved in the body's immune response.
Both water and blood plasma play important roles in maintaining the health and proper functioning of the human body.
Water and blood play important roles in the healing process of the human body. Here are a few ways in which they contribute to healing:
Hydration: Staying hydrated is important for overall health, and it can also speed up the healing process. Adequate hydration helps to keep tissues supple and pliable, allowing for proper wound healing.
Blood circulation: Blood circulation is essential for bringing oxygen and nutrients to the cells and tissues that need them to repair and regenerate. When the body is injured, blood flow to the affected area increases to help the healing process.
Temperature regulation: Water helps regulate the body's temperature, which is important for proper wound healing. A fever, for example, can help the body fight infection by raising the body's temperature, while a decrease in body temperature can slow down the healing process.
Blood plasma: Blood plasma helps to regulate blood pressure, transport hormones and vitamins, and is involved in the body's immune response. When the body is injured, blood plasma helps to form a clot at the site of injury to stop bleeding and prevent further damage.
While water and blood play important roles in the healing process, other factors such as proper nutrition, adequate rest, and appropriate medical treatment are also important for promoting healing and recovery.
Blood types are most important to know if you are needing a transfusion, but it appears that different blood types may have an impact on certain diseases.
So, considering some of the potential links to disease, you may be tempted to ask if you could change your blood type.
This wouldn’t normally happen, but it can for some people after a bone marrow transplant. This is because most of your red blood cells are made in your bone marrow. If the marrow donor has a different blood type, your blood type will eventually change to the donor's type.

Human blood is grouped into four types: A, B, AB, and O. Each letter refers to a kind of antigen, or protein, on the surface of red blood cells. For example, the surface of red blood cells in Type A blood has antigens known as A-antigens.
Each blood type is also grouped by its Rhesus factor, or Rh factor.
Rhesus refers to another type of antigen, or protein
Knowing a person's exact blood type is critical when a blood transfusion is necessary. During a blood transfusion, a patient must receive a blood type that is compatible with his or her own. If the blood types are not compatible, red blood cells will clump together, making clots that can block blood vessels and cause death.
People with Type O negative blood are considered to be universal donors because they can donate to people of any blood type.
Individuals with Type AB-positive blood are considered the universal recipients because people with that type can receive any blood type.
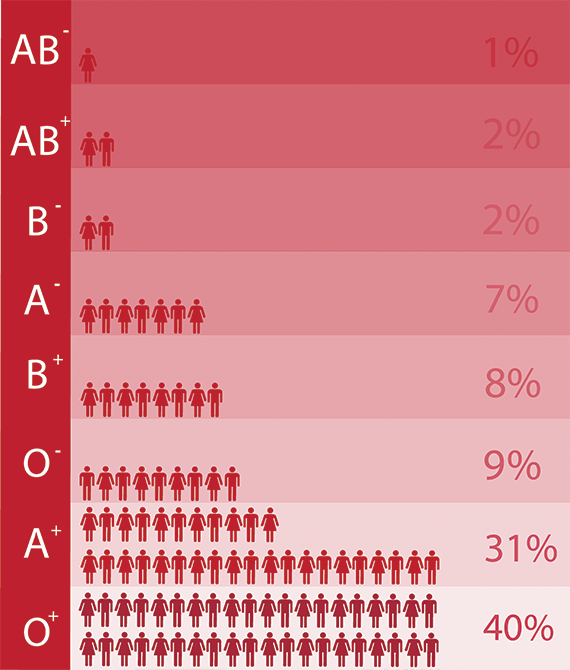
Blood Type Chart: Below is a chart listing blood types, the percentage, and the types they can donate to.
Blood type
Percent of Americans with this type
Who can receive this type?
O+
37
O+, A+, B+, AB+
O-
6
All blood types
A+
34
A+, AB+
A-
6
A+, A-, AB+, AB-
B+
10
B+, AB+
B-
2
B+, B-, AB+, AB-
AB+
4
AB+
AB-
1
AB+, AB-
A blood transfusion is the transfer of blood from one person to another. Blood that is lost through an injury, an illness, or surgery.
Matching the right types of blood is very important.
O is the most common blood type Type O blood won't provoke a response from anti-a or anti-b antibodies. AB is a rare blood type; AB negative is the rarest.
The environment can have a significant impact on the composition and function of blood. Here are a few ways in which the environment can affect blood:
Altitude: At high altitudes, the air pressure and oxygen levels are lower, which can cause changes in the blood. For example, the body may produce more red blood cells to help transport oxygen more efficiently.
Temperature: Extreme temperatures, either hot or cold, can affect blood flow and circulation. For example, exposure to cold temperatures can cause blood vessels to constrict, reducing blood flow to the skin and increasing the risk of injury. On the other hand, exposure to high temperatures can cause blood vessels to dilate, increasing blood flow and potentially leading to dehydration.
Pollution: Exposure to air pollution, such as particulate matter or ozone, can cause changes in the blood, including an increase in oxidative stress and inflammation. This can increase the risk of cardiovascular disease and other health problems.
Radiation: Exposure to ionizing radiation, such as that from X-rays or nuclear radiation, can cause changes in the blood, including DNA damage and changes in cell division and growth. This can increase the risk of cancer and other health problems.
Chemicals: Exposure to certain chemicals, such as heavy metals or toxins, can cause changes in the blood, including changes in the levels of certain chemicals, enzymes, or hormones. This can increase the risk of various health problems, depending on the specific chemical exposure.
It's important to be aware of the impact that the environment can have on the blood and to take steps to minimize exposure to environmental factors that can harm health. This may include taking precautions when traveling to high altitudes, avoiding exposure to extreme temperatures, reducing exposure to pollution and chemicals, and being mindful of the potential risks of radiation exposure.